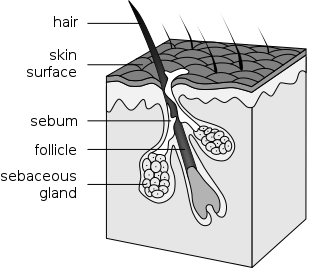
I’ve updated this post with interesting things I’ve learned in the past two years. The original post can be found here. Your skin is composed of three layers – the epidermis, the dermis, and the hypodermis or subcutis. Our main focus will be the epidermis or the outer layer of our skin. I find it interesting…